
In an NIH consortium, UW Medicine kidney researchers will study the safety and potential side effects of gene-editing as a future approach to inherited diseases
Gene editing will be tested in UW Medicine labs on kidney organoids – tiny, kidney-like structures grown from stem cells – as part of a federally funded effort to develop safe, effective genome editing technologies and therapies.
The National Institutes of Health today, Oct. 1, announced the next set of grant awards for the Somatic Cell Genome Editing consortium, created in 2018. Somatic cells make up the body’s tissues and organs, such as the lungs or blood, in contrast to reproductive cells, like fertilized eggs. Alterations made to somatic cell DNA are not passed down to the next generation.
In the latest round of SCGE funding, twenty-four grants, totaling about $89 million over four years, been awarded across the country. They will fund studies to address the promises and challenges of genome editing in the search for new treatment or cures for a number of genetic disorders.
The human genome contains thousands of genes responsible for making proteins. In many inherited disorders, a variation in the DNA code means that an important protein is not made, or is not made correctly. The missing or faulty protein could result in serious health problems. Genetic editing would aim to change the DNA to enable cells to make a sufficient amount of the proper protein.
For one of the new SCGE projects, collaborative research will take place between the University of Washington School of Medicine lab of kidney disease researcher Benjamin “Beno” Freedman, assistant professor of medicine, Division of Nephrology, and the University of California Berkeley lab of Jennifer Doudna, professor of molecular and cellular biology.
As a group, Freedman and his fellow researchers bring together expertise in kidney organoids, kidney cell biology, and kidney diseases. Their collaborators at UC Berkeley are leaders in the field of genome editing, including CRISPR-Cas9 gene editing technology to cut and paste portions of DNA in living cells.
Freedman’s lab at the UW Medicine Institute for Stem Cell and Regenerative Medicine grow stem cell-derived organoids to study how kidney diseases begin and how they might be treated. Human kidney organoids and kidney-on-a-chip technologies (in which some functions of kidneys are simulated with living cells in tiny chambers) are providing useful medical information. For example, researchers have found new molecules that can reduce the signs of disease in these laboratory models.

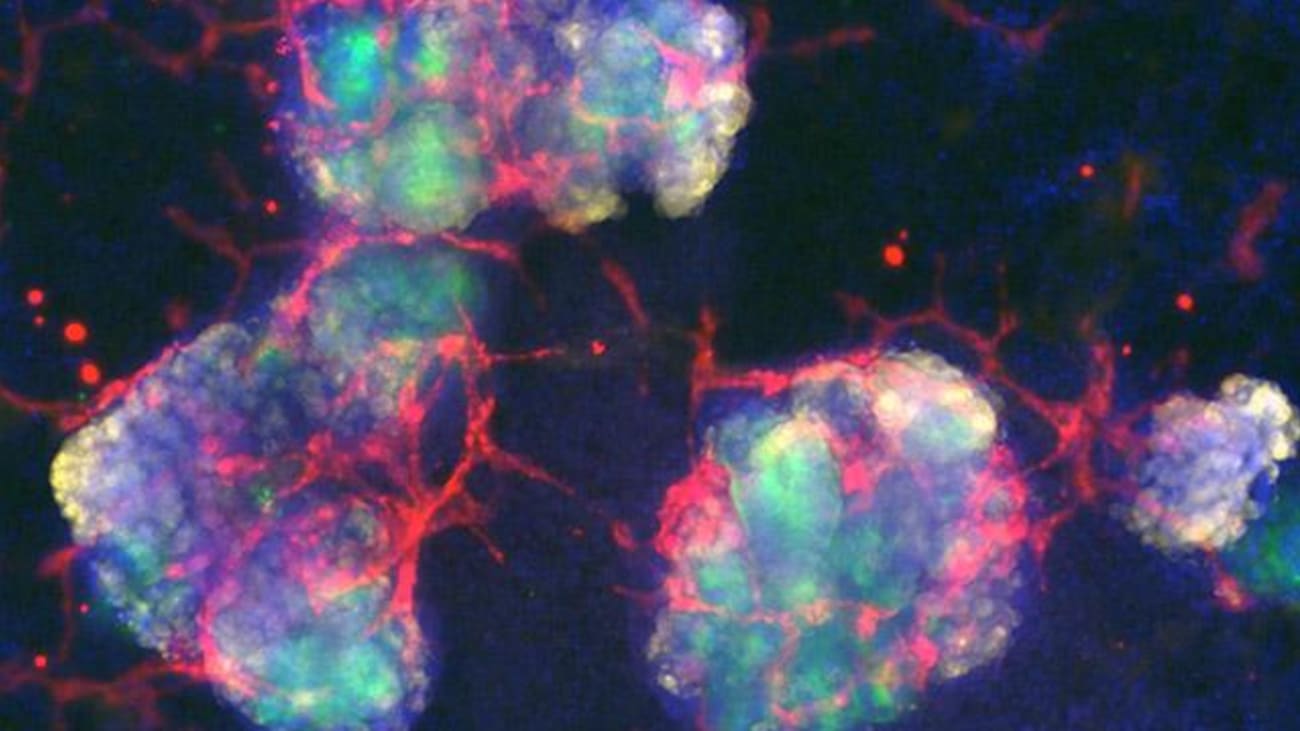
Human kidney organoid showing podocytes (red) and proximal tubules (green) developed in the Freedman lab.
Freedman explains the importance of exploring responsible gene-editing therapies for inherited kidney diseases: “Genetic kidney diseases impact more than half a million people in the United States alone. If we can learn to safely repair the mutation that causes the disease, we can offer a way to treat patients that is much more effective than any current intervention.”
Freedman emphasizes that dialysis and transplants – two of the most common treatments for kidney diseases – are expensive and hard on patients. Kidney transplants are in short supply; donor organs become available to less than 20 % of the patients who need them each year.
The shortcomings of dialysis and transplants make gene therapy an appealing area of research because it might get to the root of the problem.
One of the primary aims of the NIH-funded somatic cell genome editing explorations are to reduce the chances that gene editing produces unintended side effects that do more harm than good. In their collaborative project with UCBerkeley, the UW Medicine team will screen different gene therapies for their effects on normal kidney function and for risks of renal cancer or autoimmune disease.
“Our hypothesis is that gene editing will cause adverse effects, but that these effects are predictable and controllable,” says Freedman. “Our goal is to prove this using laboratory models like organoids and kidneys on chips so we know the approach is safe before we ever involve a human patient.”
Freedman’s lab is in the Division of Nephrology, Department of Medicine, at the UW School of Medicine, and his lab is also part of the Kidney Research Institute, a collaboration between Northwest Kidney Centers and UW Medicine.
Joining Freedman on the UW Medicine research team are Institute for Stem Cell and Regenerative Medicine colleagues Hannele Ruohola-Baker, professor in biochemistry, and Julie Mathieu, assistant professor of comparative medicine, both at the UW School of Medicine.
Ruohola-Baker will investigate how genome-editing therapies affect cell metabolism. Mathieu adds CRISPR expertise to the UW research team. Several faculty members from other departments are also on the team.
How broad are the implications of developing responsible genome-editing methods?
“This is a new paradigm for therapy development,” says Freedman. “We’re looking at the kidney. But the liver, heart, and lungs all have similar challenges. Our hope is to create a model for doing this work in human organoids, which are faster and more humane than animal models, and can be more directly compared to human patients.”
“Genome editing has extraordinary potential to alter the treatment landscape for common and rare diseases,” said Christopher P. Austin, director of the National Center for Advancing Translational Sciences and SCGE Program Working Group chair. “The field is still in its infancy, and these newly funded projects promise to improve strategies to address a number of challenges, such as how best to deliver the right genes to the correct places in the genome efficiently and effectively. Together, the projects will help advance the translation of genome-editing technologies into patient care.”
Nearly 40 million Americans have chronic kidney disease, a family of progressive conditions that can come with widespread health complications, including a higher risk for heart disease. When kidneys fail, the primary interventions, dialysis and kidney transplants, are not cures. These treatments come with significant side effects and a heavy economic burden. Medicare costs average $114 billion a year total for the care of the nation’s patients with kidney failure. Altogether, kidney disease is the ninth leading cause of death in the United States.
*Thatcher Heldring of the Institute for Stem Cell and Regenerative Medicine contributed to this news report.
